Hampshire and Isle of Wight Air Ambulance is taking part in a pioneering whole blood trial to determine whether they can reduce the number of deaths and the need for further large blood transfusions in patients with life-threatening bleeding.
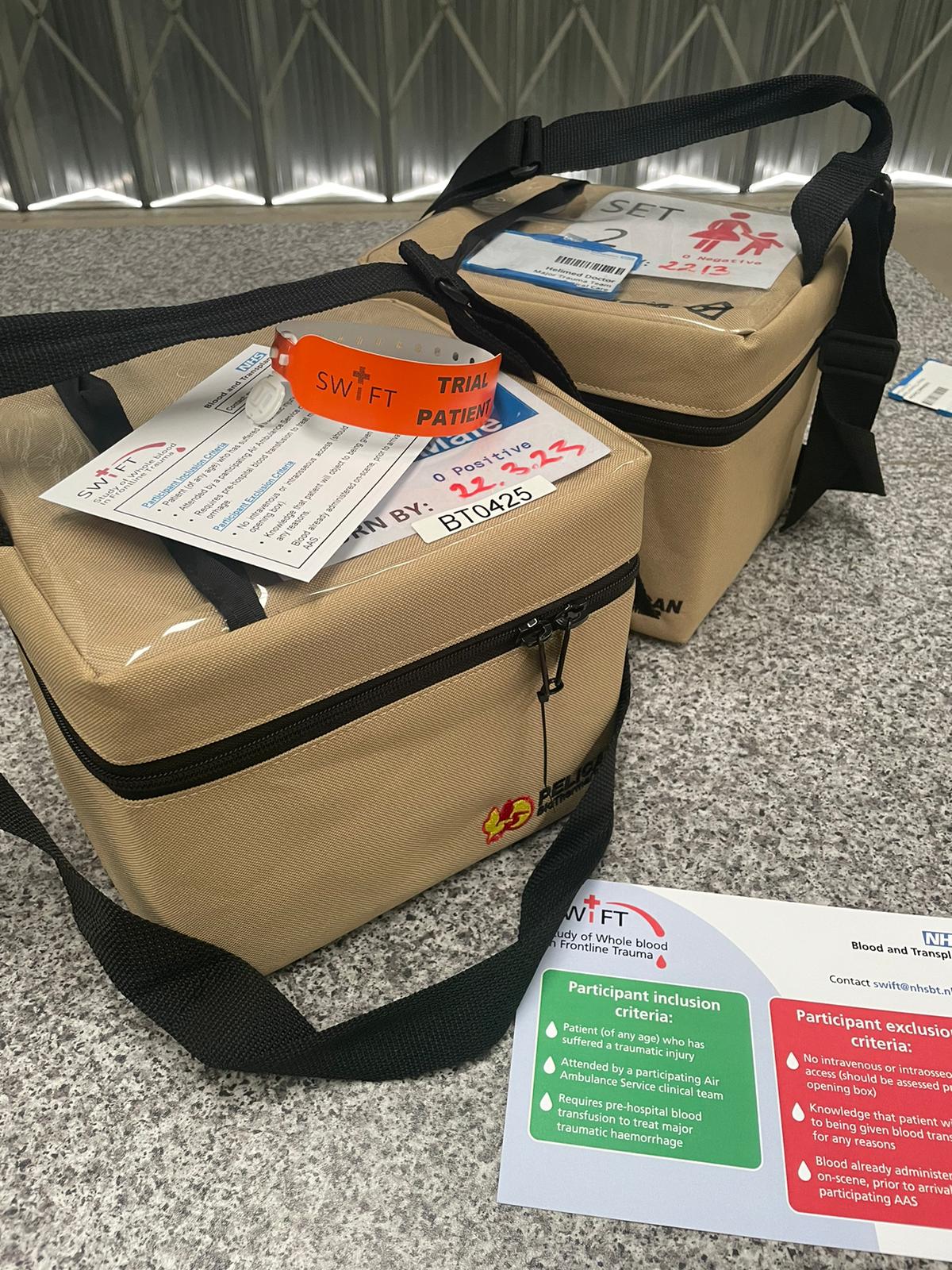
The SWIFT (Study of Whole blood In Frontline Trauma) trial, in partnership with nine other Air Ambulance charities, is due to be rolled out across Hampshire and Isle of Wight Air Ambulance on 20 March 2023.
What is whole blood?
When blood is donated, it is split into three separate components:
- Red blood cells: important for carrying oxygen around the body
- Plasma: contains essential proteins to help blood clot
- Platelets: small cells that are important for blood clot formation
This separation enables patients to receive the component that they are missing. Most patients do not require more than a transfusion of red blood cells.
In the UK, patients who are in desperate need of a blood transfusion before they arrive at hospital are given blood made up of red blood cells and plasma. Platelets, the part of the cell which helps blood to clot, must be stored at a set temperature and need constant movement to keep them oxygenated, meaning they are difficult to carry and store on an air ambulance.
Whole blood is as it is taken from the arm of the donor. It is the complete package and contains all these individual components in one bag.
Why use whole blood?
When major trauma patients bleed, they lose large quantities of all blood components required to form a blood clot. Using whole blood means the patient is getting a like for like replacement and the crew don’t need to carry separate components. It is hoped that this will reduce trauma deaths by enabling faster, more complete treatment.
All of the blood used will come from group O Rh negative donors. This is the ‘universal donor’ blood type, which is vital in emergency trauma care when there is not time to check the patient’s blood type before transfusion is started.
Dr Laura Green, co-chief investigator for SWIFT and Consultant in Haemostasis and Transfusion Medicine at NHS Blood and Transplant, said:
“The role of air ambulances in providing blood transfusions at the scene of an incident is crucial – delivering the most challenging treatments in the most challenging environments.
“Any delay to starting transfusion during traumatic blood loss can reduce the chances of survival. We hope that SWIFT will show there are logistical and procedural benefits in giving a blood transfusion of all of the components in a single bag – and ultimately improved outcomes for patients.
“Hampshire and Isle of Wight Air Ambulance exists to save lives and improve outcomes for those who are critically ill or injured in the region. We are always seeking to support clinical innovations that could help to increase the chances of survival and long-term recovery. This trial has the potential to shape the wider use of blood transfusion in out-of-hospital care and we are excited to have the opportunity to be involved from this early stage.”
Major trauma kills more than 5,400 people every year in the UK. For many of these patients, a blood transfusion before they reach hospital can be the difference between life and death. Hampshire and Isle of Wight Air Ambulance has been carrying blood and plasma on board its fleet of vehicles and aircraft since 2014.


 Donate
Donate






